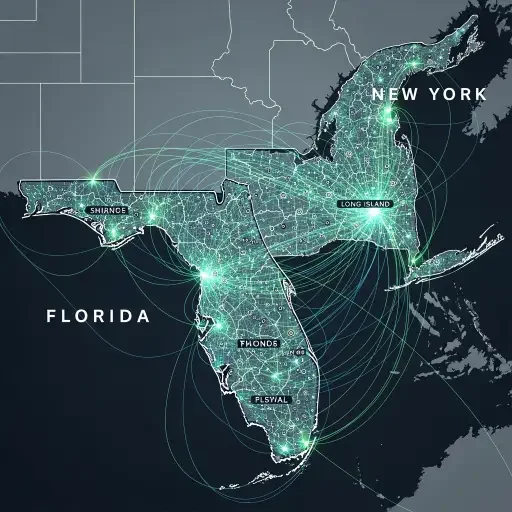
The Florida Ripple Effect
New York's budgetary brass and policy engineers woke up to a neighboring marketplace's tremor: Florida's aggressive, consumer-first privacy framework now casts a long shadow over how health data is vetted, traded, and monetized. The ripple is not just regulatory; it is economic. It redefines risk pricing, vendor diligence, and patient trust in a market built on the fragile promise of confidentiality.
Florida’s 2023-2025 privacy push, with its explicit consumer-rights calculus and explicit data-use constraints, has acted as a stress test for health data ecosystems nationwide. Florida’s move was simple in intention and brutal in application: broaden consent requirements, tighten data-sharing allowances, and empower residents with more granular control. New York, a hub of health systems, insurers, and biotech startups, watched closely. If Florida can bend the rules on how data flows, other states—New York among them—must decide whether to mirror, resist, or re-architect.
New York's Calibrated Approach
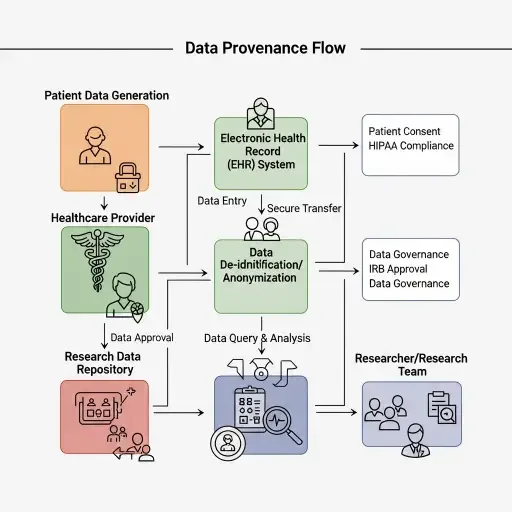
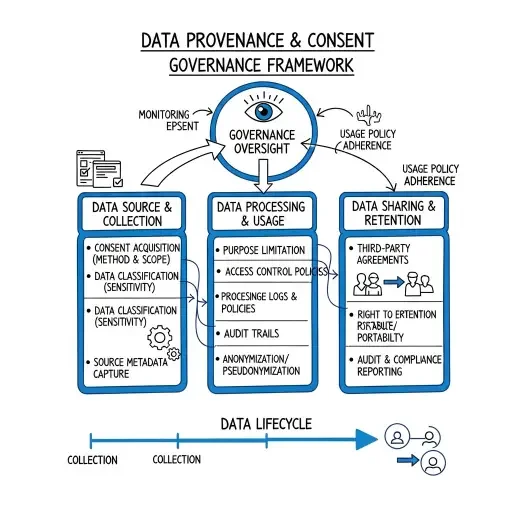
In New York, policymakers are reconciling three tensions that have long defined the data economy: patient autonomy, the commercial value of datasets, and the need for rapid health innovation. The state’s approach is not a mirror of Florida’s, but a calibration. It emphasizes provenance—clear lineage of data from origin to use—and purpose-bound sharing. It foregrounds consent not as a one-time checkbox but as an ongoing, adjustable contract between patient, provider, and platform. And it places a premium on auditable workflows: who accessed what, when, and for what purpose.
The economics of health data now hinge on governance architecture as much as on user interfaces. For hospitals negotiating risk-based reimbursement and adverse-event monitoring, the shift is palpable: data-sharing arrangements must withstand scrutiny, or value-based care strategies risk being undermined by opaque pipelines. Tech platforms, meanwhile, confront a duality: they can unlock research and precision medicine by enabling cross-institutional datasets, or they can trigger compliance frictions that raise cost and slow iteration. Investors watching this space describe a market recalibration—where the cost of data access, the premium for clean provenance, and the penalties for leakage become material levers in valuation.

Patient Agency and Data Ownership
To the patient, the questions are existential and practical: Who owns your health data when you grow older? How easily can a new app access it, and under what safeguards? How quickly can you revoke permission if you change your mind? The tension is not merely about privacy; it’s about agency—the ability to steer one’s own health narrative in a system that treats data as both passport and product.
The sector’s leaders are responding with layered defenses and deliberate disclosures. Some hospitals are accelerating role-based access controls, adding robust auditing dashboards, and embedding consent-management into the patient portal as a live, adjustable setting. Insurers are piloting data-sharing consortia with opt-in governance models that grant patients clearer visibility into use cases, from population-health analytics to drug-safety monitoring. Startups see an opportunity to build verifiable provenance tools—cryptographic attestations, tamper-evident logs, and modular data-use agreements—that can travel across markets with minimal friction. In short, the spillover is catalyzing a new coherence between patient rights and data-driven care.

The National Horizon
Yet the national horizon remains contested. Florida's posture is not a universal prescription; it is a provocation—an argument that the data economy cannot prosper without stronger protections, not in spite of innovation, but because of it. If New York’s vetting regime proves durable, other states will map similar lanes: tighter provenance requirements, more explicit consent semantics, and standardized data-use disclosures that travel with records across networks. The market’s valuation discipline will adjust to reflect the cost of assurance—risk-adjusted pricing, audit-ready data, and higher compliance layers baked into every data-sharing agreement.
This moment is less about a regulatory border and more about architectural harmonization. The health-data value chain now demands interoperable guardrails: consent tokens that travel, provenance attestations that survive aggregation, and governance dashboards that illuminate the data’s journey as clearly as its destination. In that sense, the New York experiment—quietly ambitious, almost bureaucratically exact—may become the nation’s de facto data charter.
Investor Implications
For investors, the lesson is twofold. First, data access is morphing from a raw input to a governed asset with enforceable rights and obligations. Second, the best portfolio bets will be those that fund companies delivering transparent provenance, auditable usage, and patient-centric controls—technologies that reduce friction while raising trust. The winner will be the platform that can prove, under scrutiny, that every data point has a traceable, purpose-bound lineage without compromising the speed of clinical insight.
In the end, the spillover re-centers the debate around accountability. If Florida’s playbook accelerated a national reckoning, New York’s vetting regime could codify it. The market will adapt: contracts will tighten, dashboards will brighten, and patients will notice—by a whisper and a click—how closely their data’s journey matches their own expectations.
The implicit insight remains: data is not merely a resource to be mined; it is a responsibility to be managed. The architecture of consent, provenance, and protection is no longer a nicety but a prerequisite for a sustainable, patient-first data economy.

Sources
Policy texts from Florida privacy reforms; New York Department of Financial Services and Department of Health analyses; interviews with hospital execs, data-privacy lawyers, and health-tech investors